Psychosis is a symptom caused by substance abuse, extreme stress or mental or physical illness, while psychotic disorders are defined mental illnesses. Continue reading to learn more about psychotic disorders and psychosis.
Psychotic disorders are severe mental health conditions. This group of neurological disorders changes the way a person thinks, feels and behaves. Psychosis, a shared symptom among psychotic disorders, is characterized by the presence of hallucinations and delusions.
Contrary to widespread beliefs, psychotic disorders are neither permanent nor impossible to manage on an outpatient basis. They are treatable psychiatric condition that can be controlled with medication and therapy.
Article at a Glance:
- Psychosis and psychotic disorders are neurological disorders marked by behavioral changes, delusions, and hallucinations.
- There are various types of psychotic disorders, including schizophrenia and delusional disorder.
- Chemical changes in the brain typically cause psychosis and psychotic disorders.
- Psychotic disorders are diagnosed through observation and symptom evaluation.
- People with psychotic disorders often misuse substances to find relief from their symptoms.
Comparing Psychosis and Psychotic Disorders
Psychosis is not the same as psychotic disorders. The Diagnostic and Statistical Manual of Mental Disorders recognizes psychotic disorders as diagnosable psychological conditions that can be debilitating.
People with psychotic disorders can experience a range of symptoms, including paranoia and suicidal thoughts. They have an impaired relationship with reality and may hear or see things that do not exist.
Psychosis is a symptom of several mental health disorders, including psychotic disorders. It can occur in conditions that are not psychotic disorders. For example, people with alcohol addiction can develop symptoms of psychosis even though alcoholism isn’t a psychotic disorder. Brain tumors and stroke can also result in psychosis.
Psychosis is a break from reality characterized by delusions, hallucinations and disorganized speech and behavior. While it can occur suddenly and as an isolated instance, psychosis typically arises in the course of a psychiatric disorder and rarely occurs without warning. Medical professionals refer to the onset of a psychotic episode as a psychotic break.
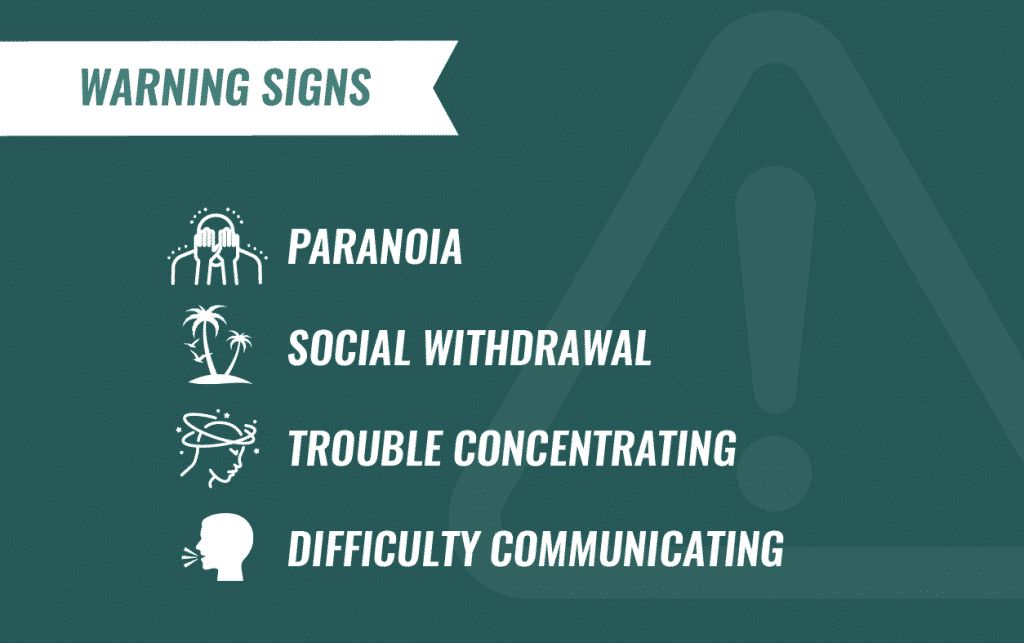
There are usually subtle warning signs of an impending psychotic break. These signs include social isolation, worsening self-care, paranoia and gradual shifts in thinking and perception. The first psychotic break in schizophrenia or other chronic psychotic disorders usually occurs in early adulthood, with an average age of 24 at first onset.
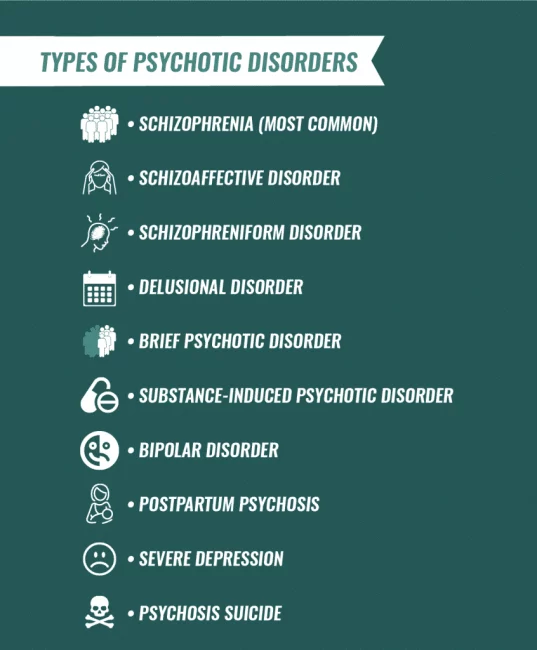
Types of Psychotic Disorders
Psychotic disorders can be short- or long-term conditions. People can experience a single psychotic episode triggered by extreme stress or other temporary changes to the brain. They can also deal with multiple psychotic breaks.
Many types of psychotic disorders exist. Schizophrenia is the most common type of psychotic disorder and is one of the leading causes of disability worldwide. But other types of psychotic conditions can also create significant health problems.
Schizophrenia
Schizophrenia comprises positive and negative symptoms. Positive symptoms add abnormal cognitive or perceptual experiences and are the symptoms most commonly associated with schizophrenia, including:
- Hallucinations
- Delusions
- Disorganized speech
- Disordered movement
Negative symptoms are those that subtract something that psychiatrically stable people normally experience or do. For example, while schizophrenia can manifest through rambling, excessive speech, it can also take form in silence.
Negative symptoms of schizophrenia include:
- Flat affect (reduced emotional expression)
- Social withdrawal (loss of interest in social activities)
- Anhedonia (reduction or loss of ability to experience pleasure)
- Avolition (reduced motivation or inability to sustain normal activities)
The way these symptoms manifest can vary from person to person.
Schizophreniform Disorder
Schizophreniform disorder is a type of short-term schizophrenia. A diagnostic criteria for schizophrenia is that symptoms must persist for at least six months. The symptoms are the same for schizophreniform disorder, but they only last for one to five months.
Schizophreniform disorder is often an early stage or precursor to schizophrenia. Over two-thirds of people develop schizophrenia after being diagnosed with schizophreniform disorder.
Schizoaffective Disorder
Schizoaffective disorder is a condition involving both psychotic and mood symptoms. These symptoms of the condition make it a particularly serious diagnosis, with a high risk of self-harm and suicide.
To be diagnosed with schizoaffective disorder, a person must experience an uninterrupted period in which they have symptoms of schizophrenia during a hypomanic, manic or major depressive episode.
Individuals with schizoaffective disorder must also experience delusions and hallucinations when no mood symptoms are present. Schizophrenic symptoms are prominent and primary in schizoaffective disorders. They are not secondary to mood disorder symptoms.
Substance-Induced Psychotic Disorder
When psychotic disorders and substance abuse co-occur, substance-induced psychotic disorder can take form. Substance-induced psychotic disorder has similar features to schizophrenia but is solely caused by the effects of drugs or alcohol.
The telltale symptom of substance-induced psychotic disorder is psychosis. Unlike other disorders involving psychosis, substance-induced psychotic disorder produces psychosis caused by using drugs or alcohol.
To be diagnosed with a substance-induced psychotic disorder, a person must experience:
- Prominent and elaborate drug-induced hallucinations
- No insight that these hallucinations are caused by drugs
- Prominent delusions that they believe are real or those that are acted upon
To be diagnosed with substance-induced psychotic disorder, symptoms must occur during intoxication or withdrawal from a substance. Symptoms cannot occur exclusively in a delirious state and cannot be secondary to a psychotic disorder that is not substance-induced.
For example, if someone experienced psychotic symptoms before they began using drugs or alcohol, it is likely that their substance use worsened or triggered an underlying condition. In this instance, substance-induced psychotic disorder is not applicable.
Delusional Disorder
Delusional disorder is a condition characterized by the presence of delusions rather than visual or auditory hallucinations. People with delusional disorder do not experience overtly bizarre behavior or significant functional impairments.
People with delusional disorder deal with false beliefs that typically involve plausible yet untrue scenarios. Individuals with this condition typically exhibit at least one of five categories of delusions:
- Erotomanic delusions (beliefs that another person is in love with them)
- Grandiose delusions (beliefs that they have special status, power, or relationships)
- Jealous delusions (unsupported beliefs that sexual partners are being unfaithful)
- Persecutory delusions (beliefs that others intend them harm or are harming them)
- Somatic delusions (beliefs that the body has been changed or had parts replaced)
To be diagnosed with delusional disorder, these symptoms cannot occur exclusively alongside a mood episode. They also cannot be cause by drug or alcohol use.
Brief Psychotic Disorder
Brief psychotic disorder occurs in individuals who experience psychotic symptoms — such as delusions, hallucinations, disorganized speech or disorganized behavior — for less than a month.
People with brief psychotic disorder return to their previous level of functioning after the brief psychotic episode has passed. This condition often occurs in response to significant increased stress or physical conditions that affect the brain.
Causes of Psychotic Disorders
Psychosis and psychotic disorders are typically caused by chemical changes in the brain. Trauma can trigger the onset of psychotic conditions, but it is rarely considered to be the sole cause.
Acute stress can provoke a psychotic break, especially when it occurs alongside a medical condition or substance abuse. But unless a person has an underlying disorder, these episodes quickly resolve and rarely recur. Psychotic episodes triggered by substance use and stress rarely develop into chronic conditions like schizophrenia.
While the specific brain mechanisms behind schizophrenia are disputed, research suggests it is linked to atypical patterns of communication between the prefrontal cortex — the part of the brain that controls judgment and planning — and the parts of the brain that control emotion and memory.
Symptoms of Psychotic Disorders
Hallucinations and delusions are telltale symptoms of psychotic disorders. However, psychotic conditions can result in several other health complications that can affect many facets of a person’s life.
Delusions
Delusions are beliefs that are not consistent with reality or social or religious norms. For example, common superstitions like worrying that breaking a mirror causes seven years of bad luck are not considered delusions.
However, believing that a malevolent entity caused a mirror to break into a specific number of shards is a delusion related to psychotic disorders. Not only is it not a shared belief, this behavior features typical delusional elements like paranoia.
Common delusions in psychotic disorders include:
- Ideas of reference (beliefs that neutral events are meaningful messages)
- Delusions of control (beliefs that an individual has been taken over by an outside force — particularly that thoughts are being inserted into or removed from the mind)
- Magical thinking (beliefs that an individual is able to control or influence the outside world with thoughts, such as being able to communicate telepathically)
Depending on the severity of disorganized thinking, delusions can be difficult to place into any of these categories.
Hallucinations
Hallucinations are perceptual disturbances that a person sees, hears, smells, feels or tastes but that do not exist. They are not exclusive to psychotic disorders and can occur in a wide range of circumstances. Hallucinations can arise alongside neurological disorders or in response to sleep deprivation.
Auditory hallucinations are the most common types of hallucinations in psychotic disorders, especially schizophrenia. This phenomenon is colloquially known as “hearing voices.” Voices may be benevolent, but more commonly are critical or threatening.
Command hallucinations can also occur, but they are not common. These are auditory hallucinations in which a voice commands an individual to commit an action that can be harmful to themselves or others.
People with psychotic disorders sometimes also experience visual hallucinations. The most common type of visual hallucination in schizophrenia is seeing a person who isn’t actually there, like a family member or religious figure. In some cases, people with schizophrenia may have frequent hallucinations of a character known only to them.
Disorganized Thinking
Disorganized thinking is typically an initial symptom of schizophrenia or another psychotic disorder.
Thought or speech distortions commonly associated with psychotic disorders include:
- Circumstantial, indirect or vague speech
- Derailment, or complete loss of topic or focus
- Illogical speech, inferential errors or odd conclusions
- Echolalia, or responding to questions or statements by repeating them
- Tangential speech, or meandering and only loosely connected thoughts
- Clanging, or speech focused on the sound of words instead of their meanings
- Neologism and word approximations, or using words in nonstandard or illogical ways
- Perseveration, or fixating on and excessively repeating particular words or statements
- Flight of ideas, or rapid topic changes based on connections that are difficult to follow
- Thought blocking, or suddenly becoming silent in the middle of goal-directed speech
- “Word salad,” or incoherent speech with no logical connection between thoughts
These symptoms range in severity. Early symptoms of psychosis are often subtle, while more severely disorganized speech patterns, like echolalia and “word salad,” typically only arise in the acute phase of a psychotic disorder.
Abnormal Motor Behavior
People with psychotic disorders often move in unusual ways. Motor disturbances are especially prevalent in people with schizophrenia, which may involve differences in the parts of the brain associated with movement.
Common types of abnormal motor behavior:
- Catatonia (restricted movement)
- Parakinesia or dyskinesia (involuntary movement)
- Parkinsonism or bradykinesia (rigidity or slow movement)
People with psychotic disorders sometimes walk with an unusual gait or put themselves in unusual postures. They may make stereotyped, repetitive movements, grimace or exhibit facial tics, or have prominent, idiosyncratic mannerisms. These individuals react slowly, stare for long periods of time or fail to avoid obstacles.
How Are Psychotic Disorders Diagnosed?
The distorted thought processes and disorganized speech of psychotic disorders can make clinical interviews difficult for acutely psychotic individuals. Diagnosing psychosis often involves observing voluntary speech and action made outside of the context of clinical interviews and confirming the presence of hallucinations and delusions.
Unfortunately, psychotic disorders are rarely detected before the first psychotic break. Negative symptoms are subtle and can signal a range of other conditions, requiring a long process of differential diagnosis to rule out other conditions with similar symptoms.
The emergence of positive symptoms of psychosis for the first time is called a psychotic break and is often accompanied by dangerous or bizarre behavior and a heightened risk of harm to self or others.
People experiencing a psychotic episode might consider harming themselves and, in rarer cases, thoughts of harming others. But they typically are unable to care for themselves or to protect themselves from harm.
Many people are diagnosed with a psychotic disorder after involuntarily committing to inpatient treatment. The behavior that leads to hospitalization is often first noticed by other concerned individuals, especially loved ones.
Who Is at Risk for Psychotic Disorders?
Risk factors for schizophrenia and other psychotic disorders include:
- Having a family history of psychosis
- Being exposed to viruses before birth
- Experiencing malnutrition before birth
- Experiencing alterations in brain chemistry
- Dealing with head trauma or brain damage
- Abusing substances in teen or early adult years
Chronic psychotic disorders are much more likely to arise in people with inherited brain differences or in those whose brains were changed by physical or chemical events early in their lives.
Psychotic Disorders Statistics
Statistics about psychosis show that while these disorders are severe, they are treatable:
- About 3 percent of people have a psychotic episode as adults
- Half of the people with schizophrenia have at least one other co-occurring disorder
- Among people who develop a psychotic disorder, 25 percent never have another episode
It is not unusual for people with psychotic disorders to misuse substances to seek relief from their symptoms. It can be overwhelming to know where to go when you or someone you care about needs treatment for psychotic and substance use disorders, but there are many targeted interventions that can help.
The Recovery Village is one of the rehab facilities that is equipped to provide treatment for psychotic disorders and addiction. To learn more about specific ways these services can help you, contact The Recovery Village today.


The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.