Like anorexia, bulimia and binge eating disorder, other specified eating disorders can negatively impact a person’s physical and mental health.
Eating disorders likeanorexia,bulimiaandbinge eating disorder (BED)deservedly receive a great deal of attention and coverage. Their ability to distort perception and endanger physical health is profound. While researching eating disorders can help prevent and treat the symptoms, no learning process is complete without exploring another, less commonly known group ofeating disorderscalled “other specified feeding or eating disorders,” or OSFED for short.
What Is OSFED?
Previously known as EDNOS (Eating Disorder Not Otherwise Specified),OSFED is amental health diagnosismedical professionals give to a people with disordered eating or distorted views of self or food. Rather than being only one condition, OSFED is a group of conditions that don’t fit into other eating disorder categories.
OSFED stands apart from other eating disorder diagnoses for two reasons:
- The disorder has symptoms that are too different from a previously established eating disorder
- The disorder mirrors some symptoms of an already established eating disorder while missing some vital diagnostic criteria
There arefive types of OSFED, including:
Treatment Can Be Life Changing. Reach out today.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
- Atypical Anorexia Nervosa:Individual meets all criteria for anorexia but still weighs within the normal or average range
- Bulimia Nervosa (of low frequency and/or limited duration):Similar to bulimia, but the person binges or overcompensates after binging less than once per week or less than three months
- Binge Eating Disorder (of low frequency and/or limited duration):Binges occur less frequently than is characteristic of binge eating disorder, and persist for less than three months
- Purging Disorder:Person purges to lose weight but does not binge
- Night Eating Syndrome:Individual partakes in repetitive, excessive food consumption after waking from sleep or after dinner
Signs & Symptoms of OSFED
OSFED tend to manifest in emotional, behavioral and physical symptoms. However, the symptoms a person exhibits can vary depending on individual differences, as well as the specific type of OSFED present.
Emotional & Behavioral Signs
Some OSFED symptoms are apparent through a person’s actions or changes in their mental state. The emotional and behavioral signs of OSFED include:
- An increased focus on dieting, weight loss and food
- Refusing to eat certain foods/ groups of foods or not eating around others
- Referring to themselves as “fat” despite not appearing overweight
- Forming rigid beliefs about food, meals and eating
- Withdrawing from friends and social activities
- Unpredictable mood swings
- Going to the bathroom immediately after eating
- Wearing loose or baggy clothing
Physical Signs
Other symptoms of OSFED affect a person’s physical health and well-being. The physical signs of OSFED include:
- Visible weight changes
- Dry skin, hair and fingernails
- Fainting or being dizzy
- Feeling cold
- Damage to teeth and gums
- Sleeping problems
- Health problems, including anemia, thyroid changes, slowed heart rate and electrolyte issues

Causes of OSFED
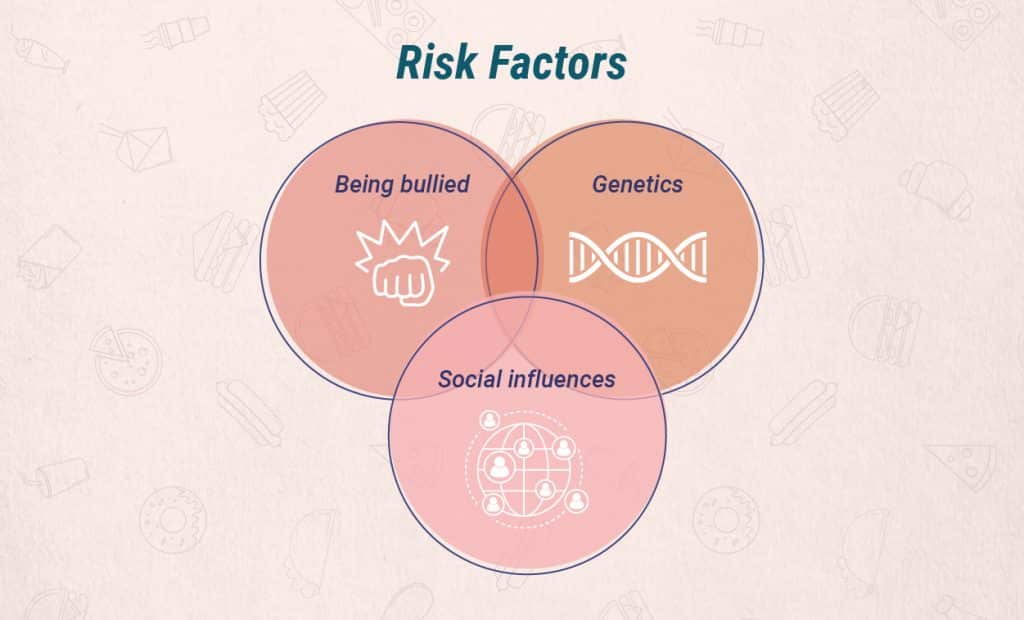
Like other eating disorders, there is no clear evidence pointing to a direct cause of OSFED. Instead, the disease is the result of the interaction between genetics, family history and environmental factors.
Risk Factors for OSFED
Without a definite cause of OSFED, experts look to warning signs and risks to study the factors that contribute to the development of OSFED. As mentioned, a person’s biology and environment can increase their risk of developing OSFED. If someone has a close family member with an eating disorder, they are more likely to have OSFED. Likewise, if a person experiences a series of situations where thinness was valued, being overweight was a problem and food carried a lot of power, they are more likely to develop OSFED.
Otherrisks factorsfor OSFED include:
- A lack of close relationships
- Being bullied or teased
- High levels of anxiety
- Perfectionistic attitudes
- Low self-esteem
- Being rigid and inflexible
- Having type 1 diabetes
- Being from a racial or ethnic minority group
Diagnosing OSFED
Diagnosing OSFEDbased on the criteria in the DSM tends to be relatively simple, as long as the individual is open and honest about their symptoms. However, people with eating disorders often minimize or deny their problems, which can make diagnosing OSFED more challenging.
Distinguishing between OSFED, typical eating behaviors and other eating disorders like anorexia, bulimia and BED can be tricky. Getting concrete details about the occurrence and frequency of binging and purging, current weight and thoughts about body image can aid in the diagnostic process.
OSFED Statistics
Though many have never heard of OSFED, the condition is surprisingly prevalent and damaging.OSFED statisticsshow:
- About six percent of people have OSFED
- At least 30 percent of people seeking treatment for eating disorders have OSFED
- Almost half of the people with OSFED have a mood disorder like depression or bipolar disorder
- About ten percent of people have a substance use disorder as well
- People with OSFED/ ENDOS are just as likely to die from the condition people with anorexia or bulimia
OSFED and Co-Occurring Disorders
Other mental health and substance abuse conditions frequently co-occur with OSFED. These co-occurring disorders can increase symptoms and complicate treatment.
OSFED often co-occurs with:
- Anxiety disorders, like generalized anxiety disorder and panic disorder
- Obsessive-compulsive disorder
- Mood disorders, including major depressive disorder and bipolar disorders
- Substance use and addiction, with alcohol use being the most common
- Body dysmorphic disorder
Treatment for OSFED
While treatment for OSFED can be complicated, recovery is always possible. Starting treatment as early as symptoms and signs are detected can help the process, but even people who have had the condition for many years can still find relief from their symptoms through professional care.
The specific type of OSFED and the presence of co-occurring diagnoses dictate treatment. Someone with OSFEDatypical anorexianervosa will undergo a different treatment program than a person with OSFED night eating syndrome.
However, while the details of treatment can vary, the essential elements of professional care will be similar. Providers will work to address all the needs of the individual simultaneously including their mental health, physical health and social health.
Helpful treatment options include:
- Medical and nutritional interventions to stabilize weight and teach healthy eating practices
- Talk therapy to help the person see how certain thoughts, feelings and behaviors maintain the dangerous disorder
- Medications, like antidepressants or anti-anxiety drugs, to aid the process and address co-occurring mental health conditions
If you are one of the many people with co-occurring OSFED and substance use disorder, now is the best time to seek treatment.Call The Recovery Village todayto start your path to recovery.









